First Response Training Guide
This training roadmap outlines the core competencies and milestones required to build knowledge and confidence as a First Response medical roleplayer.
Basic Medical Assessment (BMA) – Trainee First Response Evaluation
This assessment is designed to evaluate how a Trainee EMS handles common, low-complexity medical scenarios. It is a required step before a trainee can be promoted to EMT.
Assessment Overview
The assigned Assessor (a senior or supervisory EMS staff member) will present two scenarios from the list below. Scenarios can be described verbally or enhanced with props or other members of the EMS Staff, depending on preference and available resources:
- First-degree burns
- Closed fracture (arm or leg)
- Severe asthma attack
- Shallow laceration (e.g. knife slash or gash)
Trainee Expectations
The trainee must:
- Confidently explain their approach to assessing the patient.
- Describe appropriate treatment, including:
- Which medical tools or supplies they would use.
- How they would stabilise the patient.
- Whether or not transport to Pillbox Hill Medical is required.
- Demonstrate awareness of scene safety, patient communication, and EMS procedure.
Assessment Criteria
The Assessor should evaluate the trainee on:
- Scene Management – Maintaining control, ensuring safety, and delegating where necessary.
- Level of Care – Proper use of medical protocol and attention to patient wellbeing.
- Confidence & Communication – Showing clear, calm decision-making and professionalism throughout the scenario.
Post-Assessment
If the trainee passes the Basic Medical Assessment, they will be promoted to EMT. With continued field performance, professionalism, and consistent duty activity, they may later be promoted.
Intermediate Medical Assessment (IMA) – EMT Evaluation
This assessment is designed to evaluate how Emergency Medical Technicians (EMTs) and Hospital Nurses manage intermediate-level medical situations with emerging complexity. It marks a crucial step toward progression to Paramedic (field track) or Doctor (hospital track).
Both EMTs and Nurses must demonstrate the ability to:
- Manage care independently in moderately complex scenarios
- Recognise complications beyond surface-level injuries
- Make confident decisions about treatment, escalation, and patient flow
Passing this assessment confirms that the candidate is ready for greater responsibility and specialisation within the EMS or Hospital team.
Assessment Overview
The Assessor will present two patient scenarios, each involving:
- A clear primary injury, and
- A potential secondary complication requiring clinical judgment
Props may be used to enhance realism, but clear verbal descriptions are sufficient.
Select two scenarios from the following:
- Broken jaw with potential concussion
- Stab wound with suspected internal bleeding
- Open limb fracture with possible joint dislocation
- Gunshot wound with potential organ damage (Assessor’s choice)
Candidate Expectations
Whether you’re assessing an EMT or a Nurse, both must be able to:
- Explain their treatment plan for the obvious injury
- Identify signs of possible complications and describe how they would:
- Diagnose the issue
- Treat or stabilise the patient
- Decide on escalation (e.g., surgeon, trauma team, or advanced transport)
- Determine transport/transfer method:
- EMTs: Describe ambulance setup, patient handling, and Code call
Role-Specific Guidelines
EMTs (First Response)
- Manage care until hospital handover
- Use EMS kits effectively, maintain scene safety, and communicate clearly via radio/MDT
- Demonstrate awareness of transport priorities and basic triage
Nurses (Hospital Role)
- Provide bedside care using hospital resources
- Coordinate with doctors, surgeons, and other internal departments
- Take vital signs, initiate IVs, prep for imaging or surgery where needed
Assessment Criteria
Assessors should evaluate the candidate on:
- Medical Knowledge – Accuracy of assessment, treatment choices, and triage
- Confidence – Clear communication and professional decision-making
- Adaptability – Ability to adjust approach when complications arise
- Care Management – Proper handling of equipment, patient interaction, and documentation
Outcome
If Failed: Provide constructive feedback and recommend further reading or shadowing. The candidate should wait at least 1 week before reattempting. If Passed: Mark the candidate as certified at the Intermediate level, eligible for promotion.
Advanced Medical Assessment (AMA) - Paramedic Evaluation
The Advanced Medical Assessment (AMA) is the final step in the professional development of senior EMS and Hospital personnel. It is designed to evaluate a candidate’s leadership, clinical judgment, scene coordination, and readiness to take on supervisory responsibilities within their respective roles.
Assessment Context
This is a high-stakes evaluation scenario where the candidate must manage a critical multi-patient scene involving:
- Two unconscious suspects (10-15s) with serious GSWs, restrained and incapacitated
- One conscious Law Enforcement Officer (LEO) with a less severe injury (e.g., GSW to limb)
- Coordination with at least one agency: LSPD, SADB, or BCSO
The assessment should be staged in a controlled location away from civilian RP areas to ensure immersion and focus.
Candidate Objectives
Whether a Paramedic or Doctor, the candidate must demonstrate the following:
Scene Management & Leadership
- Secure the scene with LEO cooperation
- Maintain control and authority without escalating tensions
- Assign roles or direct available EMS/Hospital staff (if present)
- Communicate effectively with dispatch, other units, and law enforcement
Triage and Medical Care
- Accurately assess each patient and assign treatment priority
- Clearly explain treatment plans for all patients, including complications
- Manage hypotheticals: “If you were the only responder, how would you treat and transport these patients with LEO assistance?”
Operational Communication
- Execute a proper CODE 1 or equivalent call
- Provide organised updates via radio and/or MDT
- Maintain professionalism under pressure
Role-Specific Guidelines
Paramedic (Field)
- Lead scene operations and support junior EMTs
- Handle interagency cooperation and mobile treatment logistics
- Demonstrate readiness to mentor and evaluate new trainees
Evaluation Criteria
The Assessor will grade the candidate on:
- Medical Competence – Clinical accuracy and safe treatment flow
- Leadership Presence – Confidence, clear direction, and scene control
- Decision-Making – Ability to prioritise and adapt to complications
- Communication – Clarity with EMS staff, LEOs, and over comms
- Professionalism – Calm demeanor, RP engagement, and team coordination
Assessment Outcome
If Passed:
- Update the candidate’s profile
- Promote to First Response Supervisor (Field)
- Authorised to deliver (BMA) and (IMA) whilst mentor junior staff
- Eligible to take part in departmental training, assist with hiring panels, and take on more formal leadership tasks
If Failed:
- Provide detailed feedback and guidance on areas to improve
- Minimum 2 week waiting period before reattempt
- Recommend further field experience or targeted shadowing
Advanced Driving Certification 1 (ADC1) – Ambulance
The Advanced Driving Certification is designed to evaluate an employee’s ability to safely and confidently operate an emergency vehicle under pressure. This course ensures that all EMS personnel meet the high standards required for Code 2 and Code 3 responses.
- Part 1: Focuses on controlled driving, road awareness, and vehicle handling using an Ambulance in a low-risk scenario.
- Part 2: Focuses on Code 3 response (lights and sirens active) with high speed using an Ambulance in a low-risk scenario.
Part 1 (ADC1)
Instructions
- Depart from Sandy Shores Hospital on Code 2 (lights on, sirens off).
- Follow the designated route to the dock on the northern shore of the Alamo Sea.
- Upon arrival, turn around and return via the same route to Sandy Shores Hospital.

Evaluation Criteria
- No strict time limit is enforced; however, the drive must be completed at a reasonable pace.
- Trainees must demonstrate full control of the vehicle, avoiding collisions and major handling errors.
- Proper traffic awareness, reaction to surroundings, and consistent focus are expected throughout the assessment.
Part 2 (ADC1)
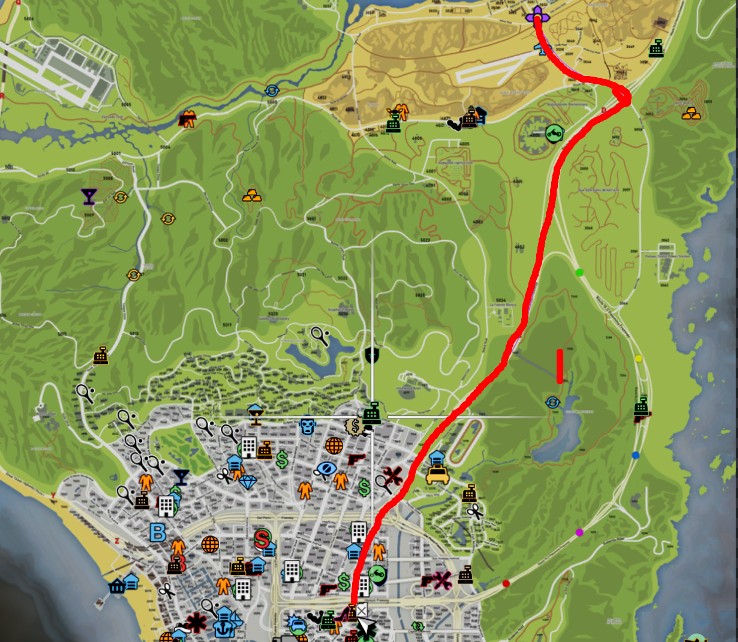
Instructions
- Depart from Sandy Shores Hospital on Code 3 (lights on, sirens on).
- Proceed to South Los Santos Gas Station entrance.
Evaluation Criteria
- There is a set time limit of 5 minutes, but the trainee is expected to drive swiftly and safely.
- The route must be completed without collisions, major handling errors, or excessive damage to the vehicle.
- Trainees should demonstrate strong situational awareness, proper use of sirens, and responsible navigation through traffic.
Advanced Driving Certification 2 (ADC2) – STX
ADC 2 focuses on the handling and operational control of the STX, a high-performance emergency response vehicle. Due to its speed , this vehicle is restricted to Paramedics and higher. It is essential that the individual operating it demonstrates full control and advanced driving judgment.
Instructions
- Trainees will begin at Sandy Shores Hospital.
- The STX will be inspected for damage prior to starting.
- If the vehicle is in acceptable condition, the assessment will proceed.
- The trainee will follow a designated red-marked course, beginning with an ascent of Mt. Chiliad via the Grapeseed approach.
- After reaching the summit, they will descend toward Paleto before returning to Sandy Shores Hospital.
- The course includes challenging off-road terrain and demands a high level of vehicle control, especially at elevation.

Evaluation Criteria
- While no strict time limit is enforced, the route should be completed at a reasonable pace, with an emphasis on safety and control.
- The trainee must avoid collisions and excessive vehicle damage.
- Given the increased difficulty of this route compared to previous certifications, some leeway may be granted — at the assessor’s discretion.
Air Rescue - Flight Assessment Certification (ARC)
The Air Rescue Certification is designed to ensure EMS personnel are fully prepared to operate ANGEL-1, our dedicated medical response helicopter. This assessment covers flight safety, emergency procedures, and practical landing skills in challenging environments.
Only those holding the rank of Paramedic or above may begin this course, as it involves handling one of the most specialised and high-risk roles within EMS.
Successful completion certifies the trainee for Air Rescue operations, pending final deployment approval by senior staff.
Orientation & Flight Safety Briefing
Before takeoff, the assessor must provide a safety overview covering essential aspects of helicopter operations:
Helicopter Safety Protocols:
- Pilots must wear secure clothing and footwear. Avoid loose garments that could interfere with rotor mechanisms or harnesses in emergencies.
- Approach the helicopter from the front or side, never from behind the tail rotor.
- All crew and passengers must remain at a safe distance until the pilot gives clearance to board.
ANGEL-1 Operational Guidelines
When considering deployment of ANGEL-1 (Air Rescue Helicopter), trainees must be trained to evaluate the situation with the following in mind:
- Urgency: Is the patient in critical condition and located in an area where ground access would be significantly delayed?
- Location: Is the patient in a remote or inaccessible location, such as an island, mountain, or rugged off-road terrain?
- Authorisation: Has the pilot received supervisor clearance for ANGEL-1 deployment? Unauthorised use is strictly prohibited.
- Purpose: ANGEL-1 is not a convenience transport. It is a costly emergency response unit and must be used responsibly.
Emergency Landing / Imminent Crash:
- Identify and aim for a safe landing zone, away from populated areas.
- Transmit a Mayday call with your location and intended course of action to alert all relevant emergency services.
- If control is maintained, use autorotation to reduce impact severity.
- Upon landing (if engine is still running), cut power, reduce throttle to zero, and secure the landing zone.
- Assess and treat crew and passengers for any injuries.
Under Attack / Small Arms Fire:
- Immediately report the threat to Law Enforcement and EMS dispatch.
- If the source is visible and flight remains viable, evade and retreat at best speed.
- If the threat is unclear or the aircraft is compromised, initiate emergency landing procedures as outlined above.
Passenger Flight Controls (Infrared and Search Lights)
In addition, the use of the EMS Chopper Cam and Night vision will also be discussed:
- ‘E’- Use Cam as passenger
- ‘Space’ - Lock on to vehicles (alt approx 100 ft)
- ‘RMB’ Right Mouse Button - Switch modes (Day, Night, Heat)
- ‘G’ - Spotlight
Part 1 (ARC) - Flight Test – Practical Evaluation
Instructions
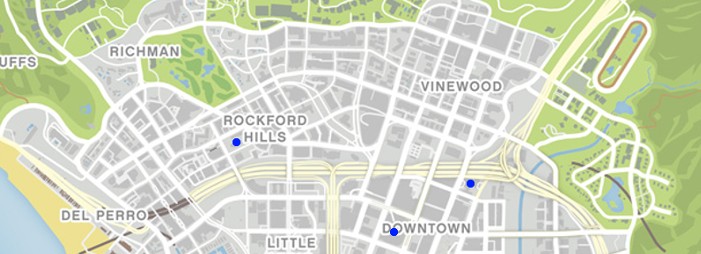
The trainee will take off in ANGEL-1 from Pillbox Heli-pad, ascending to a minimum altitude of 200-400 ft AGL. They must safely navigate to and land at the following locations:
- Maze Bank Tower
- Richards Majestic (7226)
- Then return to Pillbox
Evaluation Criteria
- Smooth takeoff and landings
- No damage to aircraft or surroundings
- Controlled flight path and situational awareness
Part 2 (ARC) - Dynamic Landing Assessment
For the final phase of certification, the assessor will choose two out of the following four locations for the trainee to respond to:
- Bolingbroke Prison
- Chumash Pier
- Vinewood Bowl
- Sandy Shores

Evaluation Criteria
The trainee must identify and utilise a safe landing zone near the selected location and perform controlled landings. Assessment Focus:
- Choice of landing zone
- Stability and control during descent
- Trainee’s rationale for selecting the landing site
Mental Health Response Training
Mental health emergencies can present in many forms, from emotional overload and panic attacks, to paranoia or extreme confusion. As an EMS provider, your response is not just medical, it’s psychological and tactical. This training manual provides the procedures, behavioral insights, and field-tested roleplay scenarios to prepare EMS units for realistic, in-character handling of psychiatric scenes.
SCENARIO 1 – THE ALLEYWAY
A concerned citizen has called in a report of a man behaving erratically in a back alley in Davis. The subject is pacing, talking to himself, and appears unaware of his surroundings. No weapons are seen. PD has not been dispatched.
Scene Objective:
- Establish a calm EMS presence
- Perform a basic behavioral and mental assessment
- Determine if the patient requires voluntary medical transport
Recommended Approach:
- Park a short distance from the subject; do not use lights/sirens unless necessary.
- Approach slowly, preferably with one unit engaging while another stays back for safety.
- Announce presence using non-threatening phrases: “Hey there, I’m with EMS. Just want to check in — are you okay?”
Patient RP Behavior Prompts:
/me paces back and forth with quick, anxious steps, eyes flicking from side to side.
/me mutters under his breath “They know I’m here… I can feel it…”
/me stops suddenly, staring at a rooftop, whispering “There… there it is again.”
/me shakes his head rapidly and clenches his fists “No, no, no — not again.”
EMS Expectations:
- Avoid loud noises or rapid movements.
- Speak clearly and calmly.
Ask simple grounding questions:
- “Can you tell me your name?”
- “Do you know what day it is?”
- “Would it be alright if we checked you out?”
Offer voluntary transport to a medical facility for further evaluation:
-“We can take you somewhere safe to talk to someone. You won’t be alone.”
Training Focus Points:
- De-escalation techniques
- Monitoring of body language
- Recognition of hallucinations vs disorientation
- Balance between professionalism and empathy
SCENARIO 2 – THE PARK BENCH
Park rangers report a man who has remained seated in Legion Square Park for several hours, motionless. He has refused to engage with anyone, and appears emotionally withdrawn. No known threats or injuries are reported.
Scene Objective:
- Assess for psychological distress or burnout
- Engage with gentle verbal interaction
- Provide a non-threatening environment for support
Recommended Approach:
- Leave vehicle parked at a distance, walk in slowly.
- Maintain a non-commanding tone. Sit or squat nearby if appropriate.
Approach with phrases like:
- “You’ve been out here a while. Mind if I sit with you?”
- “You look like you’re going through something heavy. You don’t have to go through it alone.”
Patient RP Behavior Prompts:
/me sits stiffly on the bench, arms folded, staring straight ahead without moving
/me slowly blinks, not reacting to sounds or voices at first
/me whispers “I haven’t been able to sleep. It just keeps spinning in my head.”
/me rubs his temples with shaking fingers and exhales heavily
EMS Expectations:
- Build rapport through stillness and time, don’t rush the interaction.
- Avoid pressing too hard on personal questions.
- Offer resources, warmth, and presence:
- “There’s nothing wrong with needing help. I can get you to someone who knows how to listen.”
Provide optional hospital transport:
- “We’re not here to force anything. If you’d like, we can take you somewhere quiet and safe.”
Training Focus Points:
- Handling passive emotional withdrawal
- Empathetic patient engagement
- Recognising signs of exhaustion or depressive affect
- Stillness and tone, not urgency
SCENARIO 3 – THE CLUB COLLAPSE
Security staff at a nightclub reports a collapsed civilian at the club entrance. The subject is conscious, panicked, and complaining of chest tightness and rapid breathing. The caller states the subject is “freaking out,” possibly intoxicated or suffering from a panic episode.
Scene Objective:
- Distinguish between panic attack and medical emergency
- Calm the subject and guide them through regulated breathing
- Provide non-judgmental support and safe transport
Recommended Approach:
- Approach slowly, kneel to eye level.
- Speak softly and avoid crowding the individual.
Start with supportive statements:
- “You’re okay. I’m right here with you.”
- “Try to follow my breathing. In through your nose… now out…”
Patient RP Behavior Prompts:
/me sits on the pavement, panting and gripping their chest tightly
/me gasps “I can’t breathe… I think I’m dying…”
/me trembles, tears running down their face “Everything’s closing in — I can’t stop it.”
/me claws at their shirt, trying to cool down, eyes darting wildly
EMS Expectations:
- Rule out cardiac/respiratory emergencies via vitals.
- Calm the patient using structured breathing:
- “We’ll do it together — in… 2… 3… out… 2… 3…”
If vitals are stable, explain the effects of panic attacks:
- “What you’re feeling is real, but it’s something we can treat. You’re not in danger.”
Provide transport for further evaluation:
- “We’ll take you in just to be sure. They’ll help you get through this.”